Introduction: The role for autologous stem cell transplantation (ASCT) in mantle cell lymphoma (MCL) has been recently called into question by the TRIANGLE trial, which demonstrated similar 3-year outcomes with or without ASCT among patients treated with R-CHOP/R-DHAP and 2 years of maintenance ibrutinib +/- rituximab. However, long-term follow-up is necessary to determine the durability of remissions and ascertain the true value of first-line ASCT for MCL.
Methods: This retrospective population-based study included all patients ≥18 years old who received ASCT as part of first-line therapy for MCL in the province of Alberta, Canada between 2000-2022. The primary objective was to determine freedom from progression (FFP), which was measured from the time of ASCT to disease progression. Secondary objectives were to determine progression-free survival (PFS) and overall survival (OS). FFP, PFS, and OS were estimated using the Kaplan-Meier method. Cumulative incidences of relapse and non-relapse mortality (NRM) were determined using competing risks analysis. Univariable and multivariable Cox regression was performed to identify risk factors for FFP.
Results: The study population included 141 patients with median age at ASCT of 60 years (range 34-71). At diagnosis, 130 (92%) patients had advanced stage disease, 52 (37%) had intermediate/high risk MIPI score, 35 (25%) had Ki67 >30%, 32 (23%) had B symptoms, and 17 (12%) had blastoid/pleomorphic histology. Induction protocols included R-CHOP/cytarabine combinations (n=93), R-bendamustine/cytarabine combinations (n=36), or alternative regimens (n=12). PET-defined pre-transplant disease status was complete metabolic response in 75 (82%) and partial metabolic response in 17 (18%) patients. ASCT conditioning consisted of melphalan plus total body irradiation (n=93), BEAM (n=40), or other regimens (n=8). Maintenance rituximab was received by 96 (68%) patients.
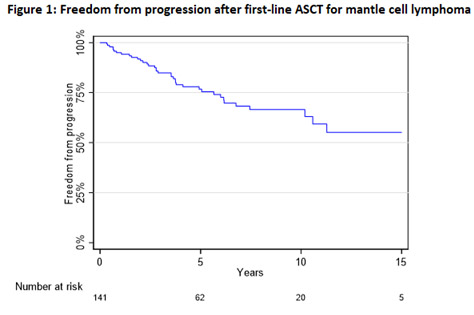
With median follow-up time 7.6 years (range 0.4-23.2), the median FFP was not reached (Figure 1) while the median PFS was 11.3 years and median OS was 14.0 years. At 8 years after ASCT, FFP was 67% (95% CI 56-75%), PFS was 57% (95% CI 46-66%), and OS was 70% (95% CI 60-78%). FFP at 8 years was 76% (95% CI 59-86%) with maintenance rituximab versus 49% (95% CI 33-63%) without maintenance rituximab (p<0.001). Multivariable analysis revealed that maintenance rituximab was associated with improved FFP (HR 0.26, 95% CI 0.10-0.72) and B symptoms were associated with inferior FFP (HR 8.45, 95% CI 2.86-25.0), whereas age, Ki67, blastoid/pleomorphic histology, and MIPI score were not significantly associated with FFP.
The cumulative incidence of relapse at 8 years was 32% (95% CI 23-41%) and the mean relapse rate appeared to decrease over time, from 4.4%/year during years 0-5 to 2.5%/year during years 6-12 after ASCT. In a subgroup analysis to evaluate the very long-term outcomes of 49 patients who underwent ASCT >10 years ago, median follow-up time was 12.5 years (range 0.4-23.2) and 13-year FFP was 40% (95% CI 26-54%), PFS was 32% (95% CI 19-46%), and OS was 54% (95% CI 35-68%). No relapse occurred >11.2 years after ASCT. Twenty patients remain alive and in remission for >10 years, 5 patients for >15 years, and 1 patient for >20 years after ASCT. There were no cases of NRM within 1 year of ASCT. Therapy-related myeloid neoplasms occurred in 3 (2%) patients.
Conclusions: This long-term follow-up study demonstrates that first-line ASCT frequently achieves durable remissions in MCL, with median PFS >11 years, a declining relapse rate over time, and notably high FFP rates among those who receive maintenance rituximab. A subset of patients experienced remissions lasting >10-20 years and may be functionally cured of their lymphoma, although additional follow-up is warranted to confirm the emergence of a plateau on the FFP curve. Given the durability of remissions and possibility of cure in some patients, longer follow-up of the TRIANGLE trial should be awaited before first-line ASCT is prematurely abandoned for MCL.
Disclosures
Owen:F. Hoffmann-La Roche Ltd, AbbVie, Astrazeneca, Beigene, Merck, Incyte, Seattle Genetics, Novartis: Honoraria. Shafey:AstraZeneca: Honoraria; Roche: Honoraria. Stewart:Gilead: Honoraria; Celgene: Honoraria; Amgen: Honoraria; Janssen: Honoraria; Roche: Honoraria; Novartis: Honoraria; Sandoz: Honoraria; Abbvie: Honoraria; AstraZeneca: Honoraria; Teva: Honoraria. Puckrin:Incyte: Honoraria; Kite: Honoraria; Beigene: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal